Why Should You Care About Consent in Healthcare?
Did you know 42% of people report symptoms without fully understanding them?
This lack of comprehension isn’t just a minor inconvenience; it is a critical breach of affected persons’ rights and might result in vital penalties for each healthcare supplier and recipients.
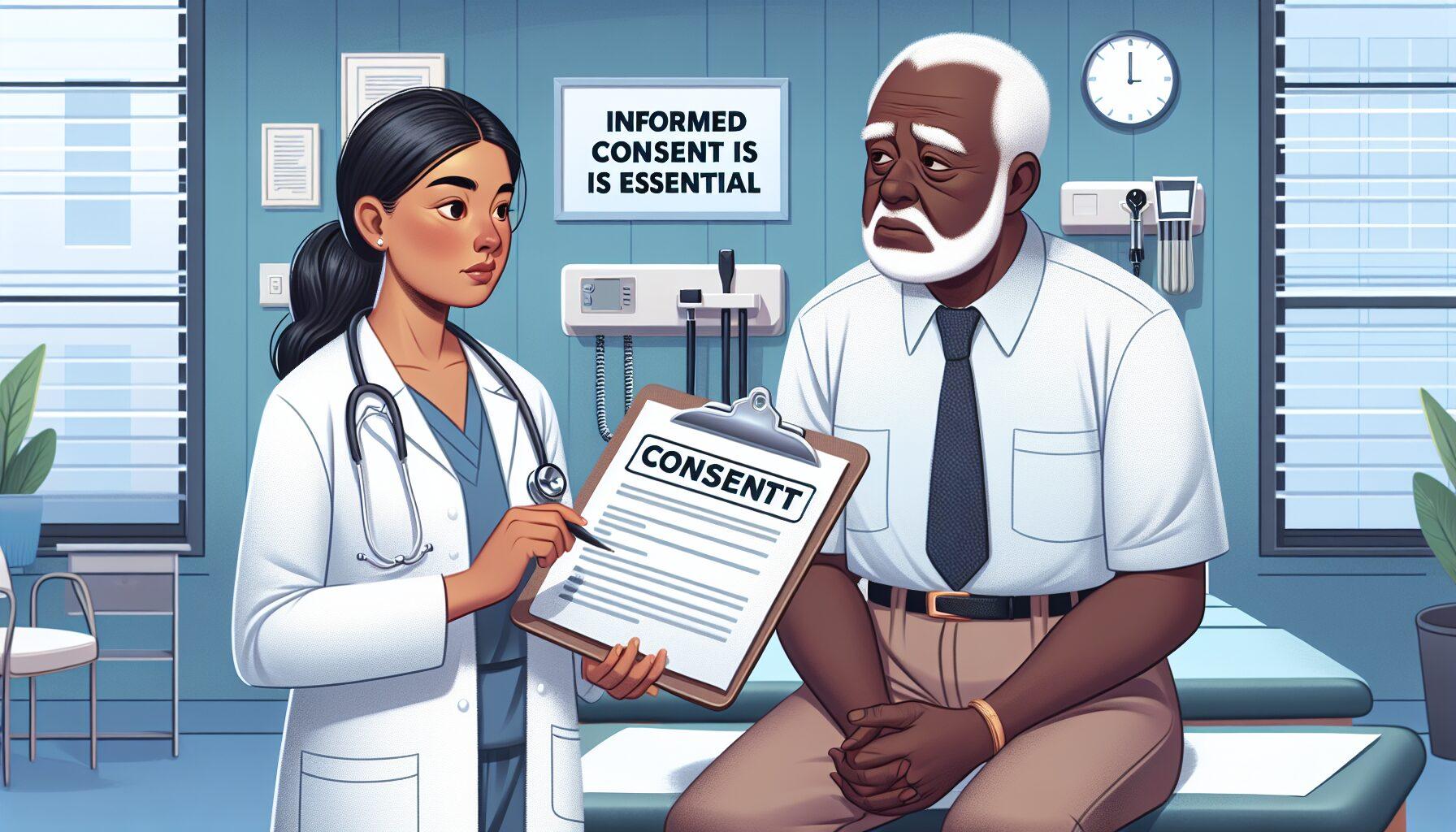
Informed consent is essential in healthcare, allowing patients to fully understand the risks, benefits, and options for any treatment. It empowers patients to take an active role in their care and fosters trust in the medical system.
Consent in healthcare extends far beyond a mere checkbox—it’s the cornerstone of ethical treatment, patient rights, and trust. With the rise of telemedicine, AI diagnostics, and digital health records, navigating consent in modern healthcare has grown increasingly complex and vital. This article delves into how evolving regulations, technological advancements, and patient advocacy affect what it means to provide informed consent in today’s medical landscape.
The Evolution of Medical Consent: From Paternalism to Partnership

From Hippocrates to HIPAA: A Brief History
The concept of medical consent has evolved significantly over time, moving from a physician-centered approach, where doctors made decisions for patients, to a collaborative model that highlights patient autonomy and informed choice.
The shift from the Hippocratic Oath, which focused on the physician’s judgment, to the modern rules of the Health Insurance Portability and Accountability Act (HIPAA) highlights society’s growing emphasis on respecting patients’ rights.
This shift mirrors broader societal changes, where increased access to information and an emphasis on individual rights have redefined trust and authority within the doctor-patient relationship.
Consent has moved from doctor-centered decisions (“doctor knows best”) to focusing on patient autonomy. The 1914 Schloendorff v. Society of New York Hospital case confirmed that individuals have the right to control their own bodies. With HIPAA (1996) and GDPR (2018), patient data rights are now a key focus.
Key Milestones in Medical Consent
1: 1947 Nuremberg Code: Established after World War II, the 1947 Nuremberg Code was enacted to address egregious medical abuses. It introduced ten ethical principles to guide scientific research, emphasizing the necessity of voluntary participant consent. This foundational document shaped modern medical ethics, underscoring the significance of informed consent and safeguarding individual autonomy in medical decision-making.
Later guidelines, like the Declaration of Helsinki (1964) and the Belmont Report (1979), built on these principles, strengthening the focus on personal autonomy and informed consent in medical ethics and research. Informed consent became essential after the WWII atrocities.
2: 1979 Belmont Report: The 1979 Belmont Report established a clear framework for conducting ethical research involving human participants, emphasizing three core principles: respect for persons, beneficence, and justice. These principles ensure that individuals are treated as autonomous agents with the right to provide informed consent, while researchers are obligated to minimize harm and maximize benefits.
The report stressed the need for fair distribution, ensuring the burdens and benefits of research are shared equally. It highlighted the importance of protecting vulnerable groups from exploitation, following ethical guidelines for human research.
3: The 2010 Affordable Care Act: Commonly referred to as Obamacare, the 2010 Affordable Care Act marked a significant overhaul of the U.S. healthcare system. Its goal was to extend insurance coverage to millions of uninsured Americans by implementing mandates, offering subsidies, and establishing insurance exchanges to enhance accessibility and affordability.
The Act, though controversial, has significantly impacted healthcare access and delivery. It highlights the need for fair healthcare services and the role of policies in improving health outcomes for diverse groups. It also promotes shared decision-making.
Understanding Modern Consent: Legal and Ethical Layers

Explicit vs. Implied Consent: What’s the Difference?
1: Explicit Consent: Explicit consent is a clear and direct agreement, usually given verbally or in writing, by a person to participate in an activity or process. It is informed, meaning the person has received all necessary details about the purpose, benefits, risks, and nature, with the chance to ask questions and consider their options.
In healthcare, specific consent is crucial for sensitive procedures, sharing private health information, or joining research studies. It ensures patients maintain control over their medical choices. Consent can be given in writing or verbally (e.g., surgery approval).
2: Implied Consent: Implied consent is a more subtle agreement that doesn’t need written or spoken confirmation. It is usually understood through a person’s actions or the situation. For example, a patient going to a clinic for treatment can be seen as giving implied consent to receive basic medical care.
Relying solely on implied consent for complex procedures or handling sensitive information can result in ethical dilemmas and potential legal challenges.
Healthcare providers must recognize the boundaries of implied consent and obtain explicit consent when necessary to uphold patient rights and professional ethics. Implied consent is typically indicated through actions, rolling up a sleeve for a blood test.
Digital Consent Forms: Revolution or Risk?
The creation of digital consent varieties in healthcare settings has been hailed as a step ahead in streamlining administrative processes and enhancing patient engagement.
By transitioning from paper-based to digital programs, healthcare providers can provide an extra interactive and informative consent experience, probably enhancing patient understanding and satisfaction. However, this shift raises issues about knowledge safety, accessibility for those not technologically adept, and the potential for oversimplification of advanced medical procedures inside digital interfaces.
Healthcare businesses must address these risks to fully unlock the benefits of digital consent without jeopardizing patient safety or trust. Telemedicine platforms like Teladoc rely on e-consent, yet 33% of users skip reading the terms (Journal of Medical Internet Research, 2022). Is convenience coming at the cost of understanding?
Debunking 3 Myths About Medical Consent

Myth 1: “Consent is merely a formality.”
Truth: Consent is far more than a mere formality; it is a critical patient right and a legal requirement. It empowers patients to make informed and active choices about their healthcare.
Without consent, any medical process poses dangers, violating moral requirements and probably the regulation, resulting in critical legal repercussions for healthcare providers and undermining the very material of patient-centered care. It’s a steady dialogue. Patients can withdraw consent mid-treatment.
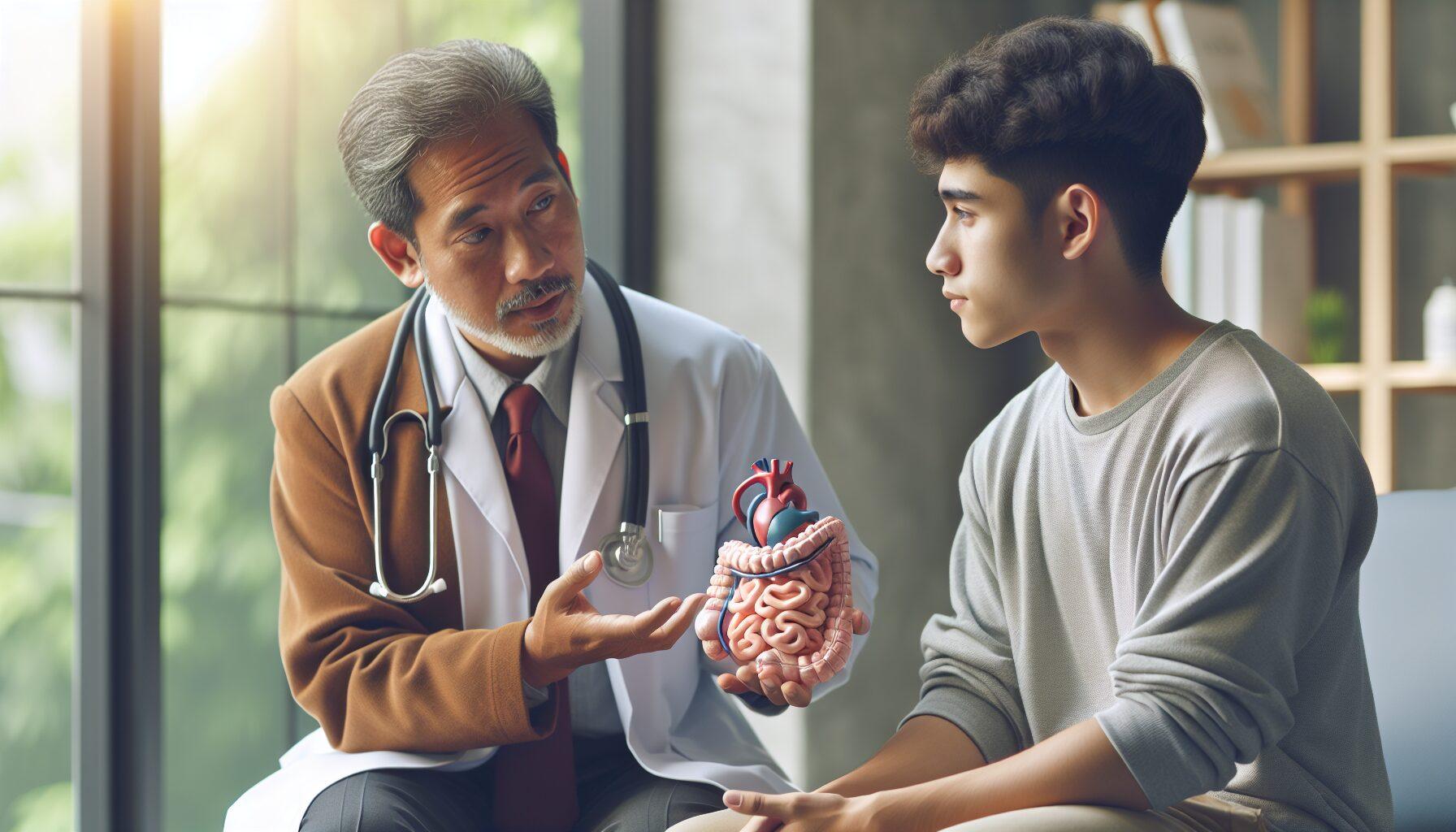
Myth 2: “Young adults don’t want consent schooling.”
Truth: Consent schooling is essential for people of all ages, however, it’s notably important for younger adults navigating new private and professional relationships and boundaries.
As younger adults transition into extra unbiased roles in society, understanding the nuances of consent becomes integral to fostering respectful interactions and avoiding dangerous conditions.
Furthermore, early schooling on these issues can lay the groundwork for healthier communication and a deeper appreciation for private autonomy and the autonomy of others. 18–24-year-olds are the least likely to ask questions throughout consultations (CDC, 2023).
Myth 3: “AI doesn’t need consent.”
Truth: AI systems must respect consent and privacy when handling personal data. Using AI for personalization still requires permission to collect, process, and use individual information.
It is crucial that builders and firms behind AI applied sciences are clear about their knowledge dealing with practices and supply customers with clear choices to opt-in or out, guaranteeing that personalization enhances the user experience without compromising individual rights. Algorithms utilizing patient knowledge nonetheless want specific permissions under GDPR.
The Legal Landscape: Who’s Protecting Your Rights?

HIPAA, GDPR, and Beyond
1: HIPAA: HIPAA, the Health Insurance Portability and Accountability Act, primarily safeguards private well-being info in the United States. It mandates that healthcare entities implement stringent measures to guard delicate patient information from unauthorized entry or breaches.
Under HIPAA, patients have the right to access their health records, giving them more control over their personal information and its use.
This framework establishes a standard for privacy in healthcare, ensuring that personalized medical services maintain confidentiality and security. While it protects health data within the U.S., it does not extend to Fitbit apps.
2: GDPR: The General Data Protection Regulation (GDPR), created by the European Union, protects personal data and privacy. It requires clear consent and gives individuals control over their information.
Under GDPR, AI personalization must respect user rights, transparent algorithms, and give customers control over their data, including opting out. This regulation sets a high standard for privacy and personalization, impacting global practices and shaping AI development. Non-compliance can result in fines of up to €20M in the EU.
Case Study: Henrietta Lacks’ Legacy
Henrietta Lacks’ story highlights key issues around personal data and AI. In 1951, her cancer cells were taken without her consent and led to medical advances. However, her family received no compensation or control over the use of her genetic material for decades. This case emphasizes the need for consent and ethics when using personal data in AI.
As AI personalization expands the limits of what is possible with knowledge, it also highlights the pressing need for robust ethical frameworks to protect individual rights and ensure that its benefits are distributed fairly.
Her cells (HeLa), taken without her consent in 1951, became the catalyst for worldwide ethical reforms. In 2023, her family achieved the right to oversee access to her genome (NYT, 2023).
Top 3 Google Searches on Consent in Healthcare
Q1: “Can a healthcare provider treat me without my consent?”
A: Consent is a key part of patient rights and ethical care. Generally, a doctor cannot treat an adult without consent unless it’s an emergency, the patient responds, and immediate treatment is needed to prevent serious harm.
This highlights the importance of informed consent, where patients are taught about the risks, benefits, and alternatives of proposed treatments, allowing them to make choices that match their values and preferences.
As the medical group continues to evolve with technological advances, the dialogue around consent is increasing to incorporate new dimensions such as knowledge, privacy, and genetic info sharing. Only in emergencies (e.g., unconscious sufferers) under “implied consent” legal guidelines.
Q2: “How do I revoke medical consent?”
A: To revoke medical consent, identify the type of consent given and the steps to withdraw it. Usually, this involves informing your healthcare provider in writing, clearly stating your decision to withdraw consent for further treatment or information sharing.
Withdrawing consent won’t affect the legality of previous treatments or data sharing but will prevent future actions without your approval. Provide a written notice, and providers must comply unless there’s an emergency.
Q3: “Does telehealth require consent?”
A: Yes, telehealth requires consent, just like traditional healthcare services. Patients must be informed about the services, the technology involved, and any data that may be collected before participating in telehealth sessions.
Healthcare providers must get patient consent to follow privacy laws and build trust for a strong patient relationship.
Consent is typically obtained online, with an electronic signature or by clicking to agree on a form before the virtual appointment starts. Telehealth platforms must collect verbal or written consent to offer their services.
The Digital Dilemma: AI, Apps, and Data Privacy
H2: Ethical AI in Healthcare: Addressing Challenges in Decision-Making
Using AI in healthcare raises important ethical issues, especially around data privacy and automated decisions. Since algorithms process large amounts of sensitive health information, strong safeguards against data breaches are essential.
Moreover, the moral deployment of AI calls for transparency and accountability, guaranteeing that selections made by artificial intelligence are truthful, unbiased, and may be scrutinized by human oversight when necessary. MIT researchers discovered racial bias in AI diagnostics—highlighting the necessity for consent about tech’s position in care (Nature, 2023).
Wearables and Data Ownership
The dialog surrounding knowledge possession intensifies as wearables grow to be extra built-in into our every day lives. These units acquire a treasure trove of private info, from physiological metrics to location knowledge, elevating issues over who actually controls this delicate knowledge.
Users have to be outfitted with clear choices to handle their privacy settings and perceive the implications of knowledge sharing, guaranteeing they maintain sovereignty over their private info amidst the rising demand for food of AI-driven personalization companies.
Who owns your Fitbit knowledge? Courts are divided. Stanford Law recommends reviewing app privacy policies yearly.
3 Practical Tips for Navigating Consent
1: Ask the “BRAN” questions: The “BRAN” questions stand for Benefits, Risks, Alternatives, and Nothing. By considering the potential advantages of sharing your knowledge, the dangers concerned, the options for offering such info, and the implications of opting out completely, people could make extra informed decisions.
It’s an easy but efficient framework that empowers customers to weigh the trade-offs of knowledge privacy versus the customization of their personal expertise.
This method encourages a proactive stance in managing one’s digital footprint, particularly as AI personalization turns into extra pervasive and complex in its capability to predict and cater to individual preferences. Benefits, Risks, Alternatives, what occurs if I say No?
2: Embracing AI personalization affords a mess of advantages, equivalent to enhanced comfort and a extra tailor-made online journey. Users can get pleasure from a discount on irrelevant content, thus saving effort and time while navigating the digital world.
However, this excessive degree of customization doesn’t come without its dangers; privacy issues loom massive as private knowledge is constantly harvested to feed the algorithms that energy these personalised experiences.
Those cautious of those dangers might search for options in the type of companies that prioritize personal anonymity or platforms that provide less focused, however extra privacy-conscious experiences.
Opting out of AI personalization might imply relinquishing certain conveniences; however, for some, the trade-off for elevated management over private info is well value it. Use an affected person advocate during advanced consultations.
3: In the realm of AI personalization, the balance between comfort and privacy is a fragile one. Users should navigate the murky waters of knowledge sharing, weighing the advantages of a tailor-made expertise the potential dangers of private info exposure.
For those that prioritize privacy, the choice to forgo AI’s predictive powers is a aware step in direction of reclaiming their digital autonomy, even when it means lacking out on the seamless interactions that AI can present. Review digital consent varieties—hover over hyperlinks to verify data-sharing phrases.
FAQs: Your Consent Questions Answered
Q1: Can minors consent to therapy?
A: A1: The capability for minors to consent to therapy varies depending on jurisdiction and the character of the therapy. Generally, minors require the consent of a father or mother or guardian; however, there are exceptions for certain conditions, equivalent to emergency care or the place minors are considered mature sufficient to grasp the implications of the therapy.
It’s essential to pay attention to the particular legal guidelines and rules in your space to make sure that consent is legally obtained and revered. Varies by state; some permit it for psychological well-being or reproductive care.
Q2: What’s “knowledgeable refusal”?
A: A2: “Informed refusal” is the idea the place an affected person has the proper to refuse therapy after being knowledgeable concerning the potential dangers and outcomes of not present process the process or treatment. It’s an essential side of the affected person’s autonomy and the moral follow of medication.
Healthcare suppliers should be sure that patients are making selections primarily based on a transparent understanding of the results, and doc the refusal process to respect the patient’s needs while additionally defending themselves legally. Patients can decline therapies after understanding dangers (e.g., Jehovah’s Witnesses refusing blood transfusions).
Conclusion: Your Voice Matters
In healthcare, patient autonomy is key. Medical professionals must ensure a patient’s voice is not only heard but respected. This means having meaningful discussions where the patient’s values and beliefs shape their care plan.
By doing this, healthcare providers not only honor individual rights but also build trust, leading to better health outcomes and greater patient satisfaction. Consent empowers. From questioning a diagnosis to declining data sharing, your choices shape the future of healthcare. Have you checked your medical consent forms this year?
Call to Action: Understanding the nuances of AI personalization in healthcare is essential for knowledgeable consent. As AI systems grow to be extra built-in into our well being administration, it is important to acknowledge the balance between personalized care and privacy issues.
By staying informed and involved in decisions about how your information is used, you help shape a healthcare system that values individual needs and ethical standards. Talk with your healthcare providers about AI’s role in your treatment, and make sure your opinions are considered in this fast-growing field.